The most significant and most common resistance mechanisms
Please click on the item you wish to explore
ESBL-s: CTX-M MULTI
ESBL (extended-spectrum beta-lactamase) production is becoming more common among Enterobacteriales.
The CTX-M-type extended-spectrum β-lactamase variants are the most frequently identified ESBLs.
ESBLs hydrolyze:
- penicillins
- 2nd, 3rd and 4th generation cephalosporins
- aztreonam
- (not cephamycins and carbapenems)
Enterobacteriales order is a normal part of the gut microbiota.
In case of inadequate hygiene, bacteria may spread from person to person through contact with colonized people and contaminated devices.
Hospital-acquired infection may be caused by Enterobacteriales:
- pneumonia
- bloodstream infection
- urogenital infection
- skin and soft tissue infection
- etc.
High risk of infection with multiresistant Enterobacteriales:
- extended hospital stay
- stay in intensive care unit
- exposure to broad-spectrum antibiotics
Carbapenemases: KPC, OXA, VIM, IMP, NDM
Carbapenemase production is more and more commonly reported in K. pneumoniae and has also been identified in other gram-negative pathogens including Pseudomonas aeruginosa.
Carbapenemases are beta-lactamases with versatile hydrolytic capacities.
Carbapenemases hydrolyze:
- penicillins
- cephalosporins
- monobactams
- carbapenems
Klebsiella with plasmid-mediated carbapenem resistance is a significant risk to hospitalized patients. The transfer of these resistance plasmids into E. coli is a significant public health threat because resistant E. coli may become part of the normal gut flora and thereby would be a source of infections in healthcare settings and the community. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3086234/)
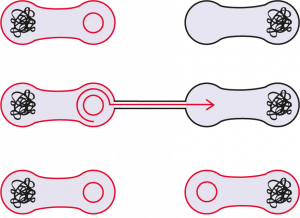
A bacterium becomes resistant through horizontal gene transfer:
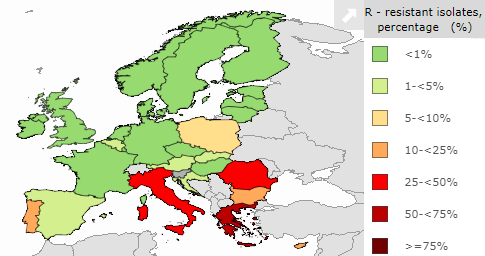
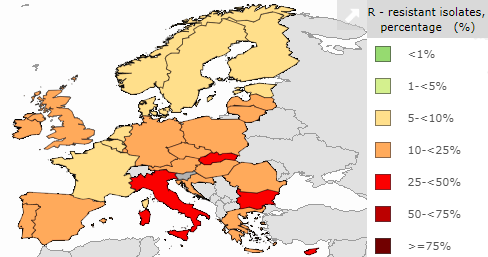
Carbapenem-resistant K. pneumoniae isolates in 2018:
VAN A/B: vancomycin-resistant Enterococci
Enterococci tend to persist in hospital environments, allowing for dissemination of resistance elements.
They are common colonizers.
Infections usually occur in immunosuppressed patients who have received multiple antibiotic treatments in the past.
Typically infection may be caused by enterococci:
- urinary tract infections
- intra-abdominal and pelvic infections
- skin and skin structure infections
- endocarditis
- central nervous system infections (rarely)
High risk of infection:
- chronic dialysis treatment
- severe underlying disease
- immunosuppressed condition
- use of invasive devices
- long hospital care
- previous or current antibiotic therapy
Van A is responsible for most of the human cases of VRE around the world and is mostly carried by E. faecium. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4521680/)
Enterococci carriers of VAN A gene are resistant to vancomycin and also teicoplanin, but the carriers of VAN B can be susceptible to teicoplanin.
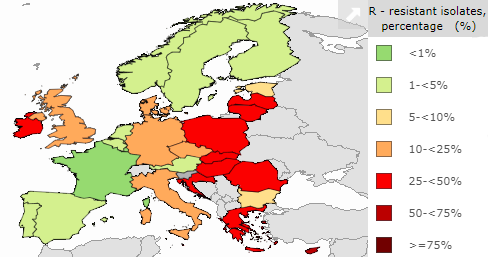
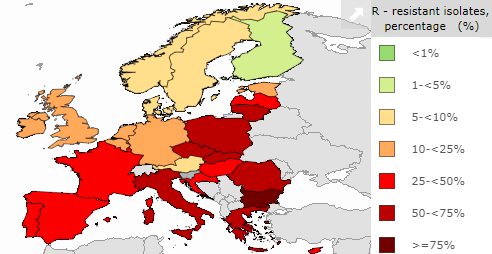
Vancomycin-resistant E. faecium isolates in 2018:
OXA-Ab: OXA-type carbapenemases in Acinetobacter sp.
Acinetobacter species are significant pathogens in hospital-acquired and healthcare-associated infections worldwide.
Acinetobacter spp. may cause:
- ventilator-associated pneumonia
- bloodstream infection
- wound infection
- urinary tract infection
A. baumannii can develop resistance to multiple classes of antimicrobial agents.
The bacterium can be found anywhere in the hospital environment, can survive on dry surfaces for prolonged periods, often causes protracted outbreaks.
Risks of infection:
- stay in intensive care units
- burn injuries
- traumatology patients
- ventilated patients
- immunosuppressed condition
- serious underlying disease (chronic lung disease or diabetes mellitus)
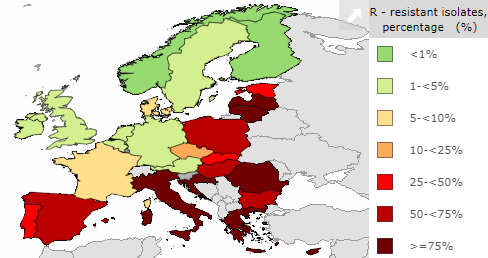
Carbapenem-resistant Acinetobacter sp. isolates in 2018:
3GC: third-generation cephalosporin resistance
3GC device for detection of determinants conferring third-generation cephalosporinase resistance (ESBLs (VEB, PER, GES, TEM, SHV), plasmid-encoded cephalosporinases (CMY, DHA)
Cephalosporins allow treating a variety of bacterial infections. Cephalosporin allergy is rare, and they generally cause few side effects. But the resistance against them is increasing:
Third-generation cephalosporin-resistant E. coli isolates in 2018:
Third-generation cephalosporin-resistant K. pneumoniae isolates in 2018:
Copyright 2020 – AMRDETECTOOL


